Obstructive sleep apnoea definition
Obstructive sleep apnoea (OSA) is a sleep disorder where breathing repeatedly stops and starts. It is associated with an increased risk of cardiovascular disease.
OSA occurs when a person’s throat and upper airway become partly or completely blocked during sleep, causing short periods where breathing stops. These periods can last up to 90 seconds, and then the individual briefly awakens. It is a problem with the mechanics of breathing.
This can happen repeatedly throughout the night, interrupting sleep and leaving the individual tired after waking. The condition is known as a ‘silent killer’, as people with OSA are often unaware they have the disorder.
OSA is one of the two types of sleep apnoea. The other, less common type of sleep apnoea is called central sleep apnoea. This occurs when the brain does not send the right signals to the muscles that control breathing.
Mild obstructive sleep apnoea
The severity of OSA is determined by how often breathing is interrupted. In mild PSA, there may be between five to 15 interruptions per hour.
Severe obstructive sleep apnoea
In severe OSA, breathing may be interrupted more than 30 times per hour. Left untreated or undiagnosed, this can have serious and life-threatening consequences.
If you experience symptoms of OSA, it’s important to see your doctor for diagnosis and to discuss treatment options.
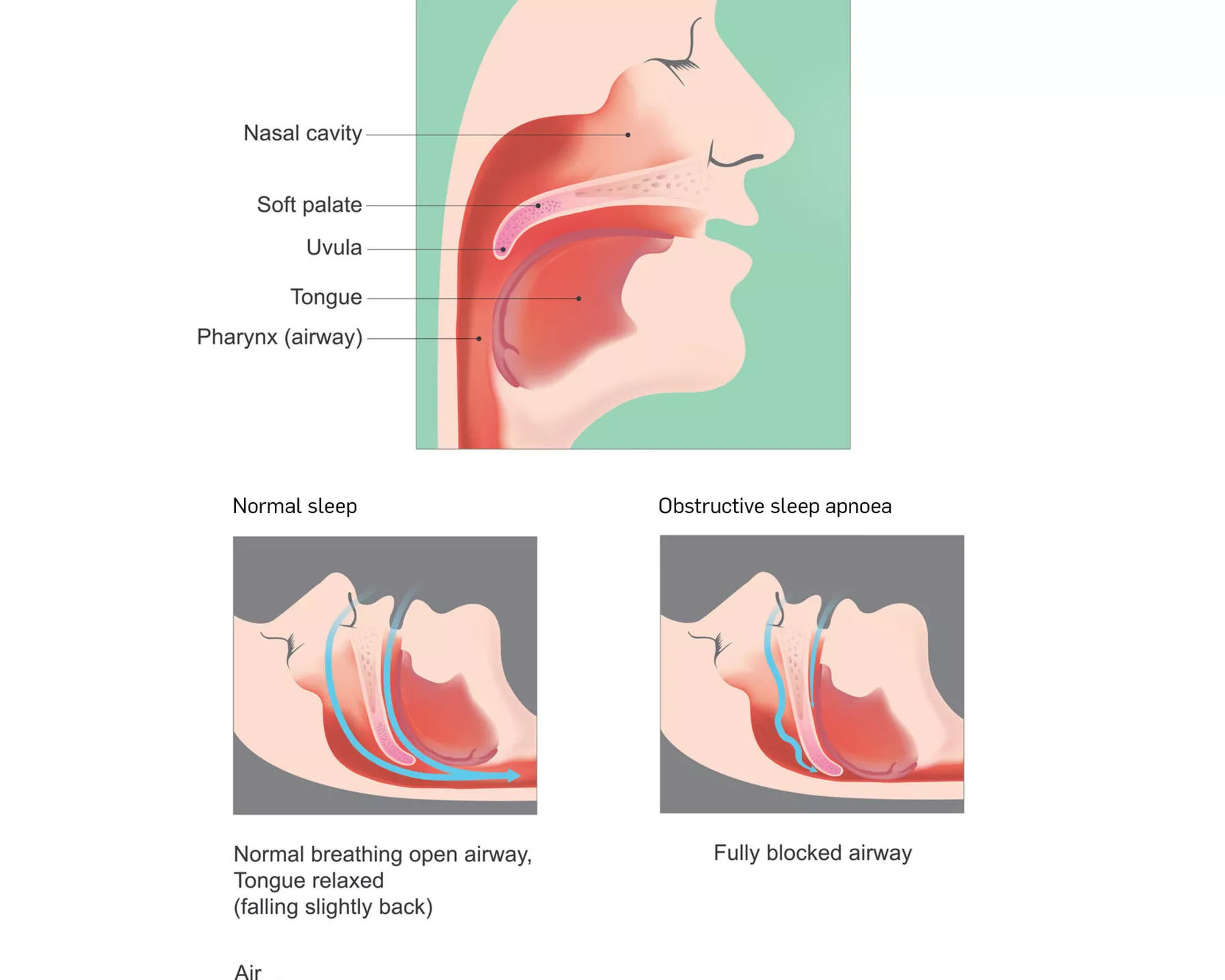
How airways are blocked in obstructive sleep apnoea
In OSA, the airways become blocked when the muscles in the back of the throat relax. These muscles support the soft palate and the uvula (triangular piece of tissue) hanging from it, as well as the tonsils, side walls of the throat and the tongue.
As the throat relaxes, the airways narrow (or even close) as the individual tries to breathe. As the individual cannot get enough air, the oxygen levels in the blood fall. This prompts the brain to briefly rouse the individual from sleep so they can reopen their airway.
When air tries to travel through the narrowed airways, it causes vibrations in the tissues at the back of the throat. These vibrations are what cause snoring sounds.
How airways are blocked in obstructive sleep apnoea
Obstructive sleep apnoea causes
The most common cause of OSA in adults is being overweight or obese. This is because excess fat in the neck and tongue narrows the throat, while fat in the upper belly can push against the lungs – both of which contribute to the airways collapsing during sleep.
However, it is now estimated that 20–30 per cent of individuals with OSA are not obese. Worryingly, people at a healthy weight who have OSA are four times more likely to develop high blood pressure and have a much higher risk of early atherosclerosis compared to obese OSA sufferers, even though healthy weight patients have less severe OSA.
Other factors that can contribute to OSA include:
- Age: As people get older, their throat muscles tend to relax more during sleep. Women should also keep an eye on their risk as they age. Premenopausal women tend to gain weight in the hips and lower body. After menopause, weight gain tends to shift to areas like the stomach, which leads to a greater chance of OSA.
- Alcohol: Alcohol makes the throat muscles relax more during sleep, leading to snoring and potentially OSA.
- Medical conditions and allergies: Some conditions may congest the upper airways.
- Facial structure: Features such as a narrow throat, round head or problems with the nose structure can contribute to OSA.
- Large tonsils and adenoids: This can cause OSA in children.
Signs and symptoms of obstructive sleep apnoea
The signs and symptoms of OSA include the following:
- pauses in breathing while sleeping
- loud snoring
- tossing and turning
- waking up gasping or choking
- having a dry mouth, sore throat or headaches upon waking
- feeling tired or not refreshed after sleep
- excessive sleepiness, fatigue or difficulty concentrating during the day
- mood changes and irritability
- high blood pressure.
Speak to your doctor if you notice these symptoms, especially if you snore loudly interrupted by periods of silence (a partner may be more likely to observe this). In OSA, snoring is usually loudest when sleeping on the back and quietens with side sleeping.
Complications of obstructive sleep apnoea
When a person stops breathing and oxygen levels drop, the body responds by releasing epinephrine (also known as adrenaline), a stress hormone. This helps the brain wake the body momentarily to breathe. When this happens over and over, adrenaline levels remain high. This can lead to high blood pressure and puts strain on the cardiovascular system.
OSA has been associated with increased risk of recurrent heart attacks, stroke, heart conditions and cardiac arrhythmias like atrial fibrillation, coronary heart disease, sudden cardiac death and heart failure.
Those with untreated moderate to severe OSA also have a higher risk of:
- diabetes
- poor memory and lack of concentration
- headaches
- mood disorders and depression
- impacted sex drive and male impotence.
As OSA can lead to excessive drowsiness and falling asleep during the day, people with OSA have an increased risk of motor vehicle and workplace accidents.
The risk of obstructive sleep apnoea
Sleep apnoea occurs in 5-15 per cent of the population.1 While it can affect anyone, it is more common in the below.
- Males: Around one in four men over the age of 30 are affected by OSA. Men are also up to three times more likely to have OSA than women, but women are more likely to have it during pregnancy and after menopause.
- Being older: OSA is significantly more common in older adults.
- Smokers: People who smoke are three times more likely to have OSA than those who do not.
- Unhealthy weight: This is the most common cause of OSA, so managing weight through eating a healthy diet and exercising regularly can help decrease risk.
- Family history of sleep apnoea: Your risk of OSA may be increased if family members have it.
Diagnosis of obstructive sleep apnoea
If you or someone you know shows signs and symptoms of OSA, such as loud snoring interrupted by pauses in breathing, speak to your doctor. Your doctor may refer you to a sleep specialist and arrange for you to have an overnight sleep study.
A sleep study is a medical test that looks at what your body does while you are sleeping. It is used to diagnose sleep disorders such as OSA. Sleep studies can be done in the home or by staying overnight at a special sleep clinic.
In the sleep study, a portable machine attached to your body will track your sleep throughout the night. It may measure brain signals, heart rate, breathing and snoring, oxygen levels and your sleep position. The results will help diagnose whether you have OSA.
Obstructive sleep apnoea treatment options
There are several treatment options for OSA, ranging from lifestyle changes to surgery, that will help you sleep more easily and may reduce the risks associated with OSA.
Treatment for mild obstructive sleep apnoea
For mild cases of OSA, your doctor may recommend the following.
- Weight loss: Losing weight may improve OSA and possible cure it, in people who are overweight or obese. Leading a healthy lifestyle with a nutritious diet and regular exercise can help manage weight and have other health benefits, such as improving cardiovascular health.
- Devices to adjust sleeping position: Sleeping on your side instead of your back may help improve OSA.
- Decreasing alcohol intake: Alcohol can be a contributor to OSA.
- Quitting smoking: Smoking increases the risk of OSA.
Treatment for moderate to severe obstructive sleep apnoea
If the treatment options for milder forms of OSA are not effective, your doctor may recommend the next line of treatment options.
- Continuous positive airway pressure (CPAP) device: This is a mask worn at night that transmits pressurised air into the airways to prevent the throat from collapsing during sleep. It is the most common treatment for OSA.
- Dental devices: These are designed to pull the lower jaw forward to create more room in the throat. They need to be fitted by a dentist.
- Surgery: If other treatments have been unsuccessful, an operation may be advised, such as one to create more room in the throat by removing tissue from the throat.
References
- Parish JM et al. Obstructive Sleep Apnea and Cardiovascular Disease. https://doi.org/10.4065/79.8.1036