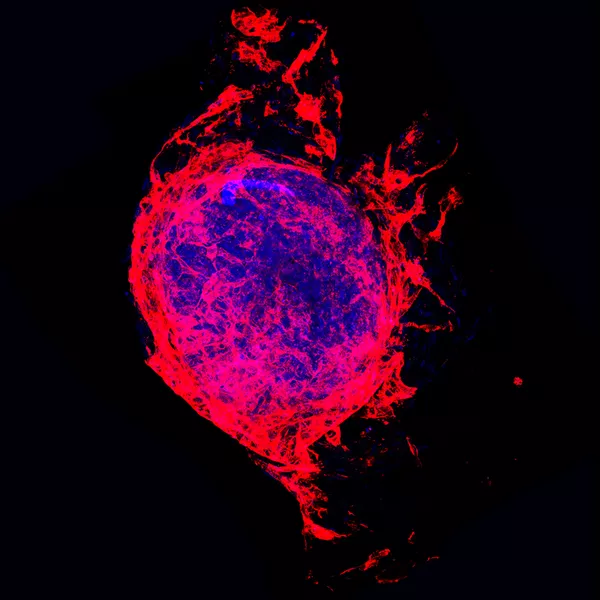
My research bridges heart disease and tissue engineering. During my PhD, one of my major projects involved creating “cardiac spheroids” or “mini-hearts” - tiny lab-grown models that closely mimic the behaviour of real human heart tissue. These models are particularly useful for studying the impact of diseases and treatments, including damage caused by chemotherapy, COVID-19, and pregnancy-related conditions like preeclampsia.
A key part of this work was developing personalised mini-hearts from patient blood samples - especially from women with preeclampsia, who face a higher risk of future heart disease. We used their blood cells to create heart cells, allowing us to examine their heart health in a personalised way. This approach could one day help predict and prevent heart problems more effectively.- a step toward better prediction and prevention.
I also explored the role of investigated acetylcholine - a brain chemical often found at lower levels in people with heart disease. In collaboration with researchers in another state, we created nanoparticles to deliver acetylcholine directly to the heart, helping to reduce damage caused by from blocked arteries or aggressive cancer therapies.
Now at HRI, I’ve built on that work and shifted focus to cardio-oncology. We’re studying how breast cancer treatments like immunotherapy and targeted therapies can unintentionally damage the heart and skeletal muscles. Using blood samples from cancer patients - with and without treatment-related heart issues - we're developing advanced mini-hearts and muscle models to replicate and better understand what’s happening in the body.