What is congenital heart disease: definition
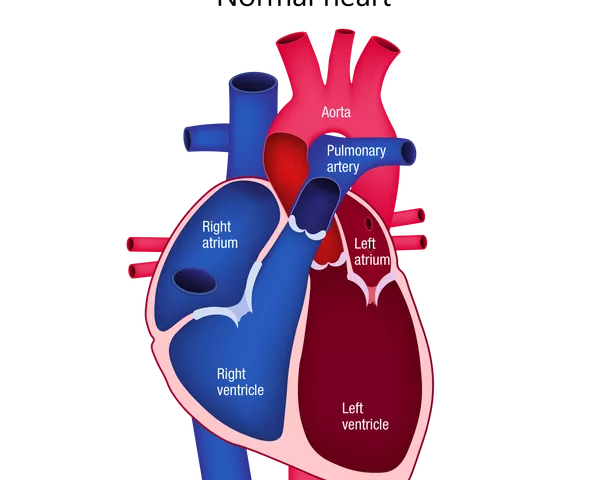
Congenital heart disease (CHD), also known as congenital heart defect, is a general term for problems with the heart’s structure that are present from birth. It is the most common type of birth defect.
CHDs can range from simple to complex and can occur in groups or alone. They can affect blood flow to the heart and the rest of the body. Some CHDs require treatment soon after birth, while some require no treatment.
CHDs can have lasting impact, so most people with CHD will require long-term monitoring of their heart condition and health. Regular monitoring as an adult is crucial, as additional treatment or intervention may be needed that was not necessary during childhood. Without proper cardiac care, these adults are at increased risk for health concerns such as reduced capacity for exercise, irregular heartbeat and late heart failure.
What are the main types of congenital heart disease?
There are many different types of CHD, which can vary from mild to severe.
Septal defects (holes in the heart)
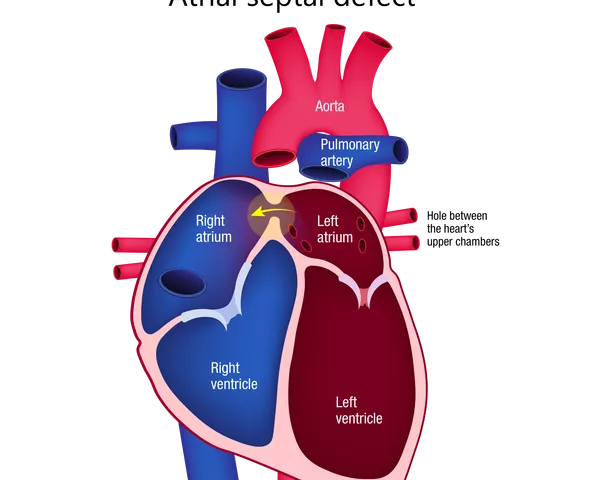
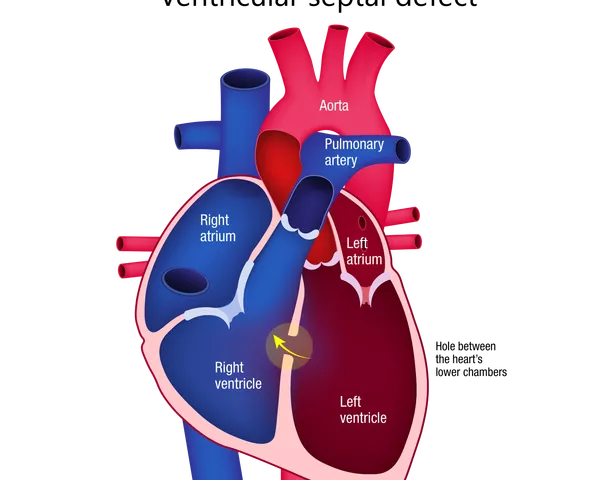
In septal defects, there is a hole in the wall (septum) between the main chambers of the heart or in one of the blood vessels. There are two types: atrial and ventricular.
Atrial septal defects are when there is a hole between the left and right upper chambers (atria) of the heart. This leads to extra blood flowing through the defect into the right side of the heart, stretching and enlarging it.
Ventricular septal defects are when there is a hole between the left and right lower chambers (ventricles) of the heart. This leads to extra blood flowing through the hole from the left to the right ventricle and to the lungs. The extra blood being pumped to the lungs forces the heart and lungs to work harder. This is a common form of CHD. Small holes often close by themselves, but surgery may be needed to close larger holes. If not repaired, over time these defects can increase the risk for complications such as heart failure, high blood pressure in the lungs (pulmonary hypertension), irregular heartbeat or stroke.
Holes can occur in the wall between the left and right atria (upper chambers), and between the left and right ventricles (lower chambers) of the heart.
Problems with the blood vessels
Defects can occur in the large blood vessels entering the heart, such as not forming properly and being too narrow, or being in the wrong position. This affects how the heart works by restricting blood flow.
These CHDs include coarctation of the aorta, patent ductus arteriosus and transposition of the great arteries.
Problems with the heart valves
Defects in the valves of the heart include the valves being too narrow or allowing blood to leak backwards. With these CHDs, the heart has to work much harder than normal to pump blood through, and extra load is placed on the heart.
These CHDs include aortic valve stenosis, Ebstein’s anomaly, pulmonary valve stenosis and total anomalous pulmonary venous return.
Single ventricle defects
Single ventricle defects are when only one of the ventricles of the heart develops properly. If not treated or repaired, these can be fatal to the baby soon after birth.
One example of a single ventricle defect is hypoplastic left heart syndrome. In this CHD, the left side of the heart does not develop properly, and the baby is born with only half a heart. The heart being underdeveloped means it cannot pump enough oxygenated blood around the body.
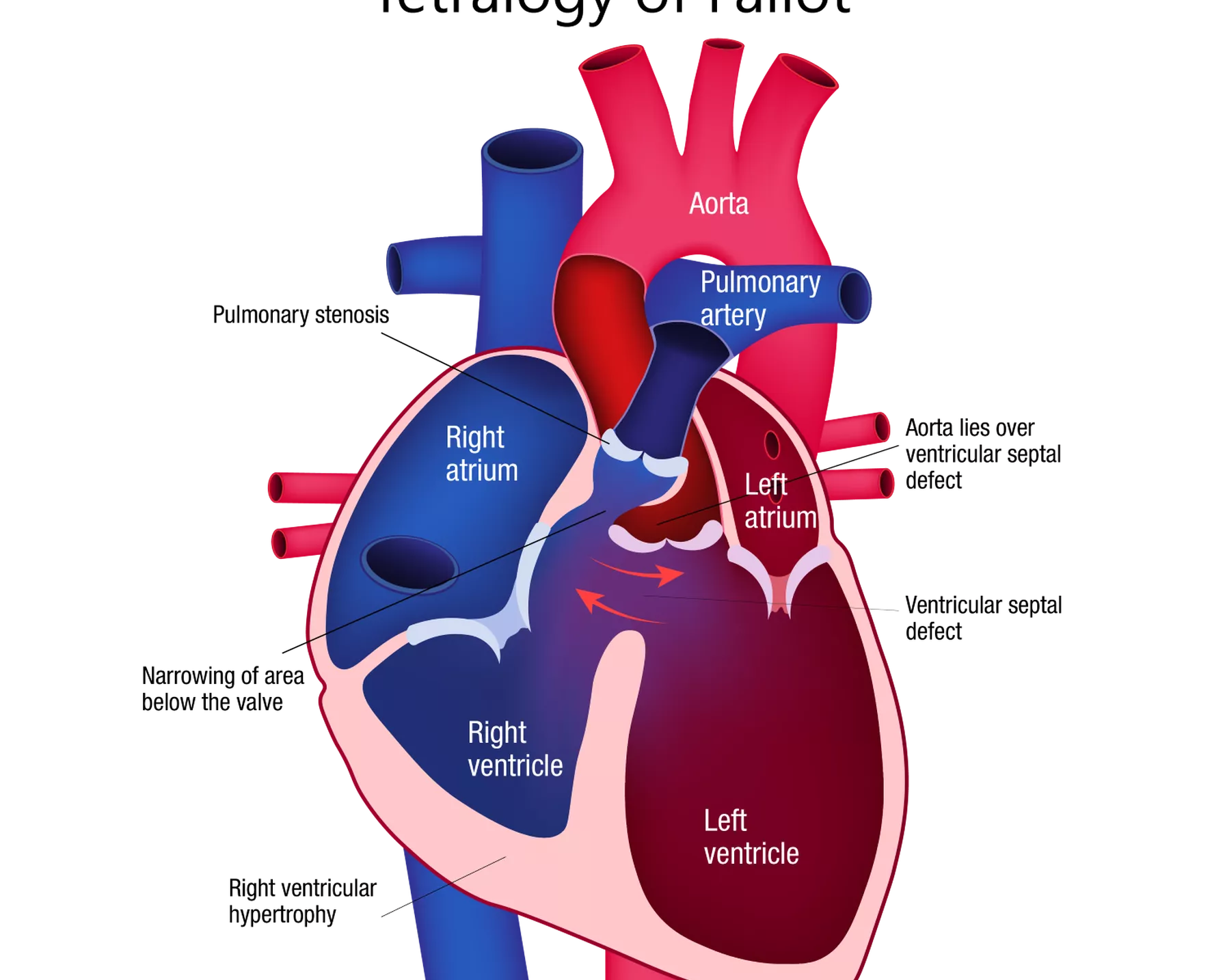
Tetralogy of Fallot
Tetralogy of Fallot is a critical CHD where there is a rare combination of four defects of the heart and its blood vessels. These include having a hole between the ventricles of the heart (ventricular septal defect), a narrowing of the pulmonary valve and main pulmonary artery (pulmonary stenosis), a thickened muscle of the right ventricle (right ventricular hypertrophy), and the aorta being in the wrong position (overriding aorta).
These defects cause the overall amount of oxygen in the blood to be lower than normal. Babies with this CHD can have bluish coloured skin because their blood does not carry enough oxygen.
Tetralogy of Fallot is a rare combination of four defects of the heart and its blood vessels.
Most common congenital heart defect
Common heart defects include ventricular septal defects, when there is a hole in the wall between the left and right lower chambers of the heart. Treatment may not be needed for small holes, but larger holes may need surgery.
Congenital heart defect: causes and risk
Congenital heart defects in CHD occur due to the heart not developing normally while the baby is in the womb. The defects can involve the walls and valves of the heart, as well as the arteries and veins near the heart. There is no known reason for CHD in most cases, although a combination of genetic and environmental factors in thought to play a part, as does family history.
Risk factors include the following.
- Diabetes: Women with diabetes have a higher risk of giving birth to a baby with CHD than women who do not. This increased risk could be due to high levels of insulin (a hormone) in the blood, which may interfere with the normal development of the baby in the womb.
- Overweight and obesity: The mother being above a healthy weight can play a part in CHD risk.
- Preeclampsia: Having this high blood pressure condition during pregnancy can increase the risk of CHD.
- Alcohol: Excessive alcohol intake during pregnancy can cause foetal alcohol spectrum disorder, which is also linked to heart defects.
- Smoking: Smoking during pregnancy increases the risk of CHD in the baby.
- Genetic conditions: Genetic health conditions that the baby inherits, such as Down syndrome, can cause CHD. About half of all children with Down syndrome have CHD. Other genetic conditions associated with CHD include Turner syndrome (which only affects females) and Noonan syndrome.
- Rubella (German measles): A rubella infection in the mother early in pregnancy can cause multiple birth defects, including CHD.
- Flu: Women who get the flu early in pregnancy are at greater risk of having a baby with CHD than women who do not.
- Certain medications: Some medications have been linked to an increased risk of CHD in the baby if taken by the mother during pregnancy. Speak to your doctor or pharmacist about reviewing the medicines that you take if you are concerned.
- Age: Older women are more likely to have a baby with CHD than younger women.
Is congenital heart disease genetic?
Genetics are a factor in CHD, with family history playing a key role.
- If either parent has CHD, the risk of CHD increases in a pregnancy. The risk is slightly higher if the mother is the affected parent.
- If one child of the parents has CHD and no other family members have it, the risk of CHD occurring in a future pregnancy is only slightly above the risk in the general population.
- If more than one child of the parents has CHD, the risk of having another child with CHD is increased.
Genetic counselling services are available to those who have, or are at risk of developing, CHD. Discuss with your doctor whether this would be a good option in your circumstances.
Congenital heart disease: symptoms
The symptoms of CHD will depend on the type and severity of the defect. Some CHDs might have no symptoms, or minimal ones.
Serious CHDs might present the following signs in the baby soon after birth or in the first few months of life:
- nails or lips tinted pale grey or blue
- irregular or rapid breathing
- swelling in the belly, legs or eye area
- tiredness or shortness of breath during feeding, leading to poor weight gain.
Other, less severe CHDs may not be diagnosed until later in childhood or even early adulthood. Signs and symptoms may include:
- easily becoming short of breath or tiring during exercise or activity
- fainting during exercise
- swelling in the hands, ankles or feet.
Speak to your doctor if you are concerned about symptoms of CHD.
Congenital heart disease diagnosis and treatment
How is congenital heart disease diagnosed?
Some CHDs can be diagnosed during pregnancy. During a routine ultrasound scan of the baby in the womb, there may be signs of CHD. In these cases, specialist ultrasounds (foetal echocardiography) may be carried out to image the developing baby’s heart to confirm the exact diagnosis. These may also be done if there is a family history of CHD or an increased risk. Not all CHDs can be detected this way, particularly mild ones.
Some CHDs are not detected until after the baby is born, such as if the newborn displays signs of CHD like bluish skin. The baby’s heart will also be checked as part of a routine examination.
Other CHDs may not be diagnosed until later in life, such as childhood, the teenage years or even adulthood.
How is congenital heart disease treated?
There is no known way to prevent or cure CHD, although there are treatments available that will depend on the type and severity of the defect.
The majority of CHDs that are mild do not need any treatment, such as small holes in the heart that repair themselves over time.
In some cases, medications may be used to relieve symptoms, improve how the heart works and treat any side effects of the CHD.
Some CHDs can be treated through cardiac catherisation, where a thin tube is threaded through blood vessels into the heart, allowing the doctor to conduct further tests or repair the defect. These procedures may improve blood flow and the way the heart works, even if they cannot always fully repair the problem. In more serious CHD cases, heart surgery may be required; some complex cases can require many surgeries over many years.
Even if the heart defect has been repaired, people living with CHD are not cured. They are likely to require regular check-ups to monitor their heart and overall health throughout their life, as they can develop other health problems over time due to their CHD.
How long can you live with a congenital heart defect?
The life span of someone born with a CHD depends on the specific CHD. Medical research has advanced heart operations and treatment such that 95 per cent of children born with CHD will now survive into adulthood, whereas in the past being born with CHD meant the baby was likely to die soon after birth or in childhood.
Even if the CHD has been treated or repaired, people living with CHD may be left with symptoms and a shortened life span.
Further research is required to improve the quality of life and life span of adults living with CHD. For example, in the past, children with CHD were discouraged from exercising due to the strain it could put on the heart. HRI is currently conducting a research project called “CH-FIT: The Congenital Heart Fitness Intervention Trial”, which is investigating whether a specific exercise program could improve the exercise ability and heart function of people living with CHD.
The impact of congenital heart disease
CHD is one of the leading causes of hospitalisation and death in infants. Around half of babies born with this disease will require surgery or another intervention. One in four babies born with a heart defect has a critical CHD – this means they need surgery or other treatment soon after birth.
In the UK, an average of 13 babies a day are diagnosed with a congenital heart defect.2
Improved diagnosis and treatment in recent years has resulted in 95 per cent of babies with CHD surviving into adulthood.
Complications of congenital heart disease
People living with CHD can be at higher risk of other health concerns, from childhood through adulthood, even if the CHD has been successfully treated. Complications of CHD include the following.
- Developmental delays: Children with a more serious CHD often develop and grow more slowly than other children. They may be smaller than other children of the same age, take longer to start walking and talking, and have learning difficulties.
- Heart infections (endocarditis): CHD can increase the risk of the heart tissue becoming infected. Bacteria or other germs can enter the bloodstream and travel to the inner lining of the heart (endocardium). If untreated, this infection can damage or destroy the heart valves or cause a stroke.
- Irregular heartbeat: This can be caused by a CHD or scar tissue in the heart from surgery to treat CHD. The heart may beat too fast, too slowly or in an irregular rhythm.
- Respiratory tract infections: People living with CHD have a higher risk of developing an infection of the lungs and airways.
- High blood pressure in the lung arteries (pulmonary hypertension): Some CHDs send more blood to the lungs than normal, causing the blood pressure in the arteries connecting the heart and lungs to be much higher than it should be. This can eventually cause the heart muscle to weaken and sometimes fail.
- Heart failure: In heart failure, the heart cannot pump enough blood around the body to meet the body’s needs. It may develop if the heart defect is significant, and it can occur shortly after birth or as a complication later in life.
- Blood clots: CHD can increase the risk of a blood clot forming inside the heart and travelling through the circulatory system to the brain, where it could block blood supply and cause a stroke, or to the lungs, where it can cause a pulmonary embolism.
How is HRI fighting congenital heart disease?
HRI’s Clinical Research Group is conducting research into CHD, with a focus on young adults living with CHD. The Group runs one of the largest Adult Congenital Heart Disease Clinics in Australia, at the Royal Prince Alfred Hospital, Sydney. Research conducted by the group includes projects designed to improve quality of life and exercise capacity for people living with CHD; improve health outcomes in CHD for young adults, their families and the health system; and establish a unique National Congenital Heart Disease Registry and develop it into a world-class resource with profound translational impact.
References
- Australian Institute of Health and Welfare 2019. Congenital heart disease in Australia. Cat. no. CDK 14. Canberra: AIHW.
- British Heart Foundation. UK Factsheet July 2020.